
The Challenge of Compliance
There’s nothing more important than patient safety when it comes to the use of medical devices. In an ongoing effort to lower the risk for patients, the U.S. Food and Drug Administration (FDA) has recently implemented a new regulation requiring that all medical devices sold within the United States be documented and tracked.
For medical device manufacturers, this new UDI (Unique Device Identification) regulation requires compliance beginning as early as September 24, 2014. That’s a short amount of time to not only gather the 62 points of data required for each unique device, but to submit them in the correct format to the FDA’s new Global Unique Device Identifier Database (GUDID) for each and every unique product, product version, and product configuration. Although the regulation will first be enforced for Class III Medical Devices, Class II and Class I devices will follow suit in the coming years.
Are you prepared to comply? Underestimating the scope and scale of this regulation could put your U.S. sales at risk. Read more to learn what’s required and how you can achieve UDI compliance.
- The Regulatory Reality
- How to Approach It
- Gauge Your Readiness
The Complexities of UDI Compliance
The stakes can literally be life or death if medical device manufacturers fail to adhere to the Food and Drug Administration’s (FDA) new Unique Device Identification (UDI) rule. Compliance is complicated, and the costs of non-compliance are severe. With deadlines for many devices less than a year away, manufacturers must implement compliance processes and technology now.
Few products depend more on accurate identification than medical devices.
Take, for example, an implanted pacemaker. If it malfunctions, it’s critical for the information in the adverse event report to match the manufacturer’s product identification system – lest the adverse event go unreported. The same need holds, just as urgently, for a product recall sent from the pacemaker’s manufacturer to the doctor, hospital, or patient. An inability to identify the device affected by the recall could have potentially disastrous results for patient health.
In a five-year period, the U.S. Food and Drug Administration received an average of just less than half a million adverse event reports involving medical devices each year. Annually more than 280,000 of these reports, on average, noted injury to the patient. In an average of nearly 18,000 reports per year, the patient’s outcome was death.
This harsh reality raises the stakes for consistency and accuracy in product identification. When misidentification occurs, it’s most often due to a distribution company, hospital, or clinic renumbering the product. The need to correctly identify the medical device—both when conveying vital product information from the manufacturer to the field and when reporting problems back to the manufacturer—could hardly be more urgent.
Every minute lost to product misidentification can put a patient’s life on the line.
Commanding the Complexities of UDI Compliance

So Much to Do… in So Little Time
By now, the UDI reality for medical device manufacturers should be firmly setting in: They must put in place a complete UDI compliance solution by the government’s imposed deadline or risk being deemed non-compliant.
It’s a tall order. The UDI rule’s requirements are numerous and complicated. The right compliance solution should enable the manufacturer to:
- Gather, submit, and track UDI data. The manufacturer must collect and properly format data for submissions. They must monitor FDA responses and quickly resubmit corrected data, when needed. Accurate data must be stored for recalls and audits.
- Govern the UDI submission process. The solution must support 21 CFR Part 11 with secure electronic records, technology validation, and fully documented training – all in a scalable architecture to meet emerging global UDI requirements.
- Manage and synchronize UDI changes. The manufacturer must keep all UDI submissions current with product line updates. The solution must collect and control UDI data from across the organization. Preconfigured templates and workflows, along with procedures for change and configuration management, are needed.
A manual approach to UDI compliance will likely be an unacceptable drain on resources. How about developing an automated UDI compliance solution internally? Conceivably this is an option. But as manufacturers who have considered it are increasingly coming to conclude: The do-it-yourself approach may bring many more risks than rewards.
What is the alternative?
Executive Scorecard: UDI Compliance Readiness
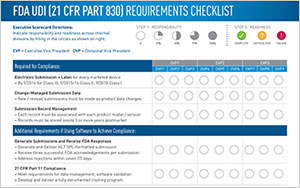
This scorecard is designed to help executives responsible for UDI compliance determine their teams’ responsibility and readiness for both the practical and regulatory requirements of achieving compliance with the FDA UDI ruling. To help executives gain a perspective on how to meet these requirements across the various divisions and teams at their organization, this scorecard outlines both the regulatory and the practical requirements of achieving FDA UDI compliance whether a software or a manual solution will be employed.
Gauge your readiness

Watch the on-demand webcast to learn the practical demands that any technology solution must fulfill in order to meet the UDI regulatory requirements with minimal risk to business operations. In addition, see how PTC executive scorecard can help you measure your company’s UDI compliance readiness in time for the FDA’s UDI submission deadline of September 24, 2014.